In this post, we gathered the essential needs for patients and their families who suffered from coronavirus to learn how to self-manage after COVID-19 covering the following aspects curated from WHO: Managing breathlessness, exercising after leaving the hospital, managing problems with your voice, managing eating, drinking, and swallowing, managing problems with attention, memory, and thinking clearly, managing activities of daily living, managing stress and problems with mood and when to contact a healthcare professional.
Your family and friends can help support you as you recover, and it may be helpful to share this post with them.
Managing breathlessness
It is common to experience breathlessness after being in the hospital. Losing strength and fitness while you were unwell, and the illness itself can mean you become breathless easily. Feeling breathless can make you feel anxious, which can make breathlessness worse. Staying calm and learning the best way to manage your breathlessness will help.
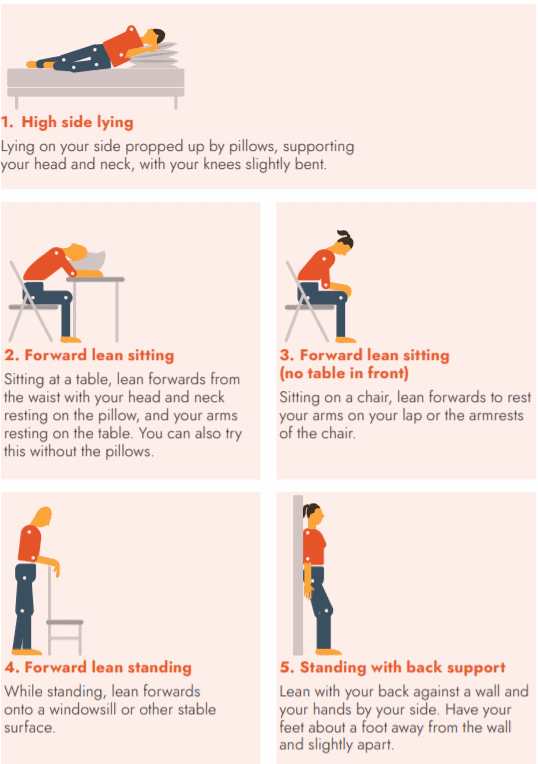
Your breathlessness should improve as you slowly increase your activities and exercise, but in the meantime, the positions and techniques below can also help to manage it.
If you start to feel severely short of breath and it does not get better with these positions or techniques, contact your healthcare professional.
Positions to ease breathlessness
These are some positions that may reduce your breathlessness. Try each of them to see which one/s helps you. You can also try the breathing techniques described below while in any of these positions to help ease your breathing.
 WHO/EURO:2020-855-40590-54773
WHO/EURO:2020-855-40590-54773
Breathing techniques
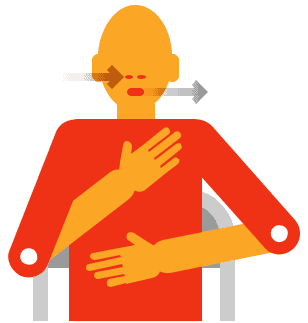
Controlled breathing
This technique will help you to relax and control your breathing:
- Sit in a comfortable and supported position
- Put one hand on your chest and the other on your stomach
- Only if it helps you to relax, close your eyes (otherwise leave them open) and focus on your breathing
- Slowly breathe in through your nose (or mouth if you are unable to do this) and then out through your mouth
- As you breathe, you will feel the hand on your stomach rise more than the hand on your chest
- Try to use as little effort as possible and make your breaths slow, relaxed, and smooth
Paced breathing
This is useful to practice when carrying out activities that might take more effort or make you breathless, like climbing the stairs or walking up a hill. It is important to remember that there is no need to rush.
- Think about breaking the activity down into smaller parts to make it easier to carry out without getting so tired or breathless at the end
- Breathe in before you make the ‘effort’ of the activity, such as before you climb up a step
- Breathe out while making the effort, such as climbing up a step
- You may find it helpful to breathe in through your nose and out through your mouth
Exercising after leaving the hospital
Exercise is an important part of recovery after a severe COVID-19 illness. Exercise can help to:
| • | Improve fitness | • | Improve your thinking |
| • | Reduce breathlessness | • | Reduce stress and improve mood |
| • | Increase muscle strength | • | Increase confidence |
| • | Improve balance and coordination | • | Improve your energy |
Find a way to stay motivated with your exercises. Keeping track of your progress with a diary or exercise ‘app’ on your phone or watch may help.
Exercising safely
Exercising safely is important, even if you were independent with your mobility (walking) and other exercises before becoming sick. It is particularly important if you:
- Had difficulty with your mobility before going into hospital
- Had any falls before going into hospital or during your time in hospital
- Have any other health condition or injury that may put your health at risk with exercising
- Have been discharged from hospital on medically prescribed oxygen
In these cases, you may need to exercise with someone else for safety. Anyone on additional oxygen MUST discuss their use of oxygen during exercise with a healthcare professional before starting.
These simple rules will help you exercise safely:
- Always warm-up before exercising, and cool down after exercising
- Wear loose, comfortable clothing and supportive shoes
- Wait at least an hour after a meal before exercising
- Drink plenty of water
- Avoid exercising in very hot weather
- Exercise indoors in very cold weather
If you feel any of the following symptoms, do not exercise, or stop exercising, and contact your healthcare professional:
- Nausea or feeling sick
- Dizziness or lightheadedness
- Severe shortness of breath
- Clamminess or sweating
- Chest tightness
- Increased pain
Remember to obey physical distancing rules when exercising outdoors, if these exist where you live.
Exercising at the right level
To work out whether you are exercising at the right level, think about speaking a sentence:
- If you can speak the whole sentence without stopping and are not feeling breathless, then you can exercise harder
- If you cannot speak at all, or can only say a word at a time and are severely breathless, then you are exercising too hard
- If you can speak a sentence, pausing once or twice to catch your breath, and are moderate to almost severely breathless, then you are exercising at the right level
Remember that it is normal to feel breathless when you exercise, and it is not harmful or dangerous. Gradually building your fitness can help you become less breathless. In order to improve your fitness, you should feel moderate to almost severely breathless when you exercise. If you do feel too breathless to speak, you should slow down or stop to rest until your breathing feels more controlled.
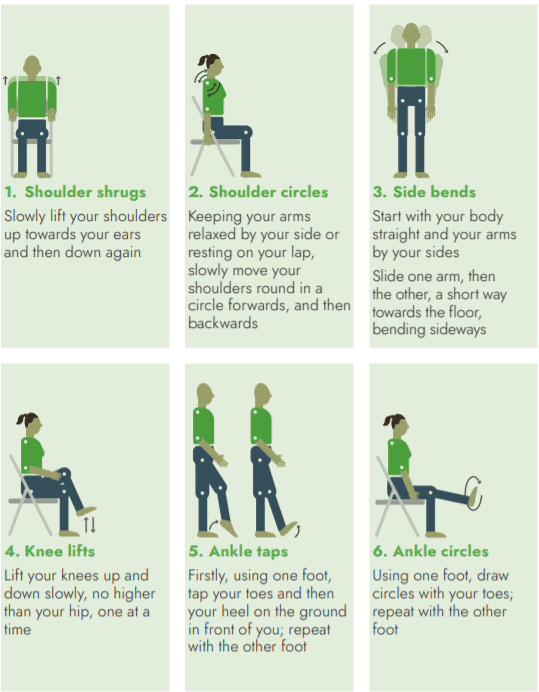
Warm-up exercises
Warming up prepares your body for the exercise to prevent injury. Your warm-up should last around 5 minutes, and in the end, you should feel slightly breathless. Warm-up exercises can be done sitting or standing. If you do your warm-up in standing, hold on to a stable surface for support if needed. Repeat each movement 2-4 times.
WHO/EURO:2020-855-40590-54773
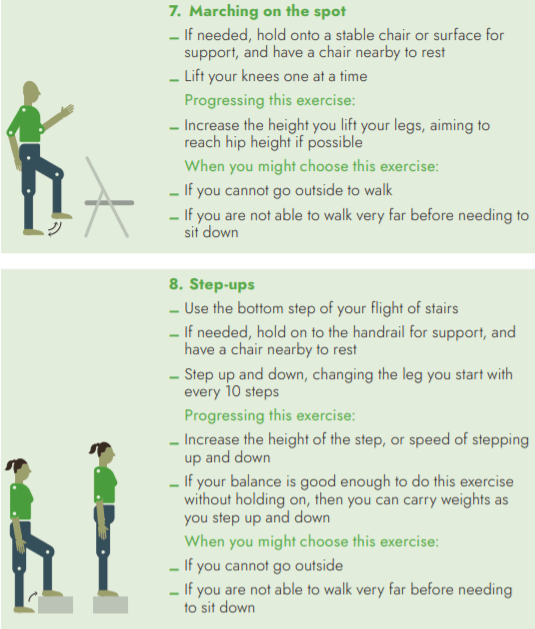
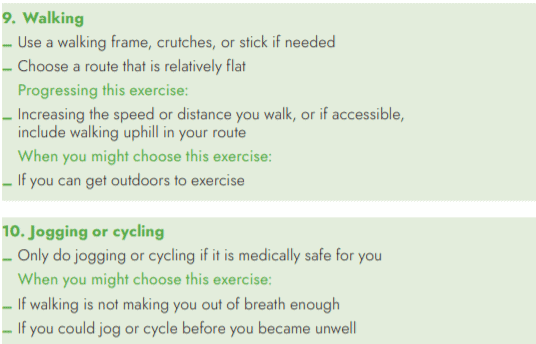
Fitness exercises
You should aim to do fitness exercise for 20-30 minutes, 5 days each week.
Some examples of different types of fitness exercises are described below, but any activity that makes you feel moderate to almost severely breathless can be counted towards your fitness exercise. Time your fitness exercise and gradually build up the amount of time you can manage. This may be in small increases such as an additional 30 seconds or 1 minute of activity. It may take a while to return to the level of activity you were normally able to do before you became unwell.
Examples of fitness exercises:
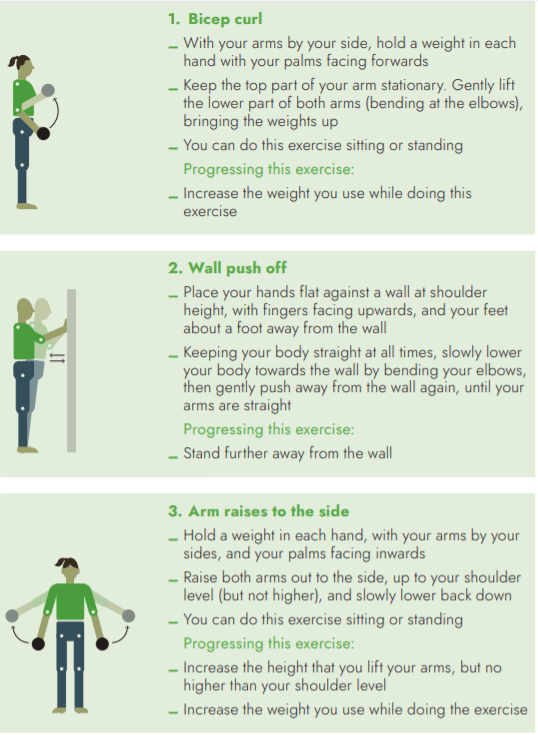
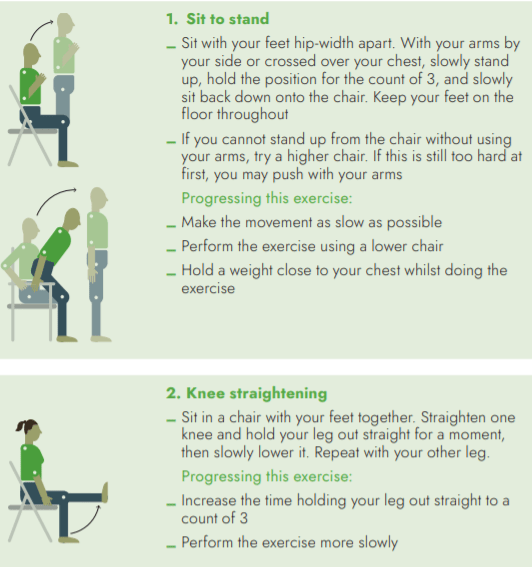
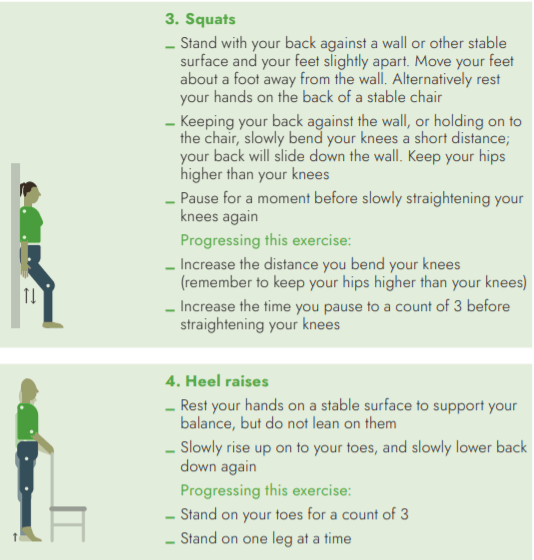
Strengthening exercises
Strengthening exercises will help improve muscles that have become weaker as a result of your illness. You should aim to do three sessions of strengthening exercise each week. Strengthening exercises will not make you feel breathless in the same way as fitness exercises. Instead, your muscles will feel like they have worked hard.
You should aim to complete up to 3 sets of 10 repetitions of each exercise, taking a short rest in between each set. Do not worry if you find these exercises hard. If you do, start with a smaller number of repetitions in each set and build up to achieving sets of 10. As you get better with the exercises, use heavier weights to make your muscles work harder. You can use tins of food or bottles of water as weights.
Some strengthening exercises for your arms and legs are described below, which can be done in sitting or standing. These can be done in any order. Keep a good posture, with your back straight and your tummy tucked in, and complete the exercises slowly.
Remember to breathe in as you prepare to do the hardest part of the exercise and breathe out as you make the effort.
Examples of strengthening exercises for your ARMS
Examples of strengthening exercises for your LEGS
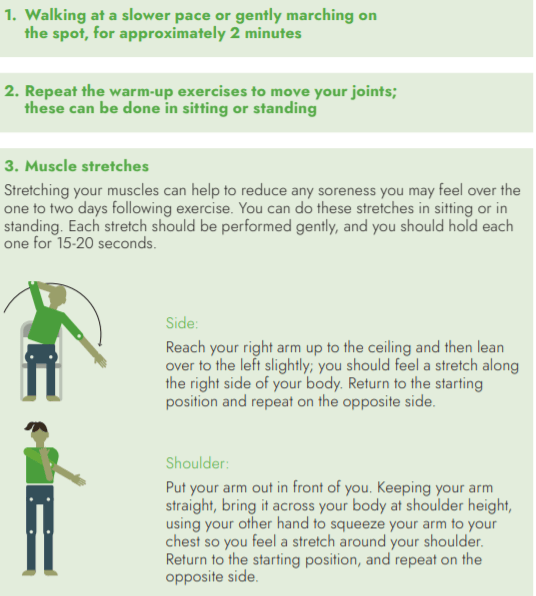
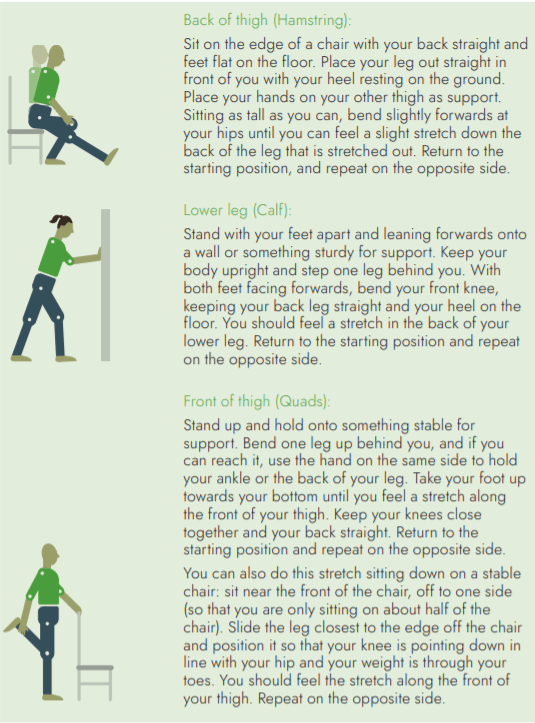
Cooldown exercises
Cooldown exercises allow your body to return to normal before stopping the exercise. Your cool-down should last approximately 5 minutes, and your breathing should be back to normal by the end. Try working through all these suggestions, but if you cannot manage all the exercises or stretches, do the ones that you can.
Managing problems with your voice
Sometimes people may have difficulties with their voice after being ventilated (having a breathing tube). If your voice is raspy or weak, it is important to:
- Keep talking when it is comfortable. You will need to keep using your voice to make progress. If you get tired while speaking, take breaks, and let your friends and family members know that you need to pause and rest your voice during conversations.
- Do not strain your voice. Do not whisper as this can strain your vocal cords. Try not to raise your voice or shout. If you need to get someone’s attention, try making noise with an object.
- Take rests. If you run out of breath while talking, be careful not to work harder. Stop and sit calmly, while focusing on your breathing. Try the breathing strategies described earlier in this leaflet. Do these until you feel ready to speak again.
- Try humming to yourself to practice using your voice, while being careful not to strain.
- Use other ways of communicating, such as writing, texting, or using gestures, if talking is difficult or uncomfortable.
- Sip water throughout the day to help keep your voice working.
Managing eating, drinking, and swallowing
If you were ventilated with a breathing tube while you were in the hospital, you may notice you have some difficulty with swallowing food and drink. This is because the muscles that help with swallowing may have become weak. Eating well and drinking water/juice is important to your recovery.
Paying attention to swallowing is important to avoid choking and lung infections. This can happen if food/drink goes the wrong way and gets into your lungs when you swallow.
If you experience difficulty swallowing, these techniques may help:
- Sit upright whenever you eat or drink. Never eat or drink while lying down.
- Remain upright (seated, standing, walking) for at least 30 minutes after meals.
- Try foods of different consistencies (thick and thin) to see if some foods are easier to swallow than others. It may help to choose soft, smooth, and/or moist foods at first, or to chop up solid foods into very small pieces.
- Concentrate when you eat or drink. Try to have your meals in a quiet place.
- Take your time when eating. Take small bites of food, take single, small sips of drink between mouthfuls of food, and chew well before you swallow.
- Make sure your mouth is clear before taking another bite or sip. If you need to, swallow again.
- Eat smaller meals throughout the day if you get tired of eating full meals.
- If you cough or choke or your breathing becomes difficult when you eat and drink, take a break to recover.
Eating healthily is very important to your recovery, especially when you are weak or have been on a ventilator. Brushing your teeth after every meal and staying hydrated will help to make sure your mouth stays healthy.
If eating and drinking continue to be difficult, contact your healthcare professional.
Managing problems with attention, memory, and thinking clearly
It is very common for people who have been severely unwell, especially those who had a breathing tube in hospital, to experience new difficulties with attention, remembering things, and thinking clearly. These difficulties may go away within weeks or months, but for some people, they can last longer-term.
It is important for you and your family to recognize if you are experiencing these difficulties, as they can have an impact on your relationships, daily activities, and your return to work or education.
If you experience these difficulties, these strategies may help:
- Physical exercise can help your brain recover. While this may be difficult if you are experiencing weakness, breathlessness, or fatigue, try gradually introducing gentle exercise into your daily routine. The fitness and strengthening exercises described earlier in this leaflet are a good place to start.
- Brain exercises, such as new hobbies or activities, puzzles, word and number games, memory exercises, and reading may help. Start with brain exercises that challenge you but are achievable and increase the difficulty as you are able. This is important for keeping you motivated.
- Prompt yourself with lists, notes, and alerts, such as phone alarms, that can remind you of things you need to do.
- Break down activities into individual steps to avoid feeling overwhelmed. Some of the strategies listed below for managing activities of daily living may also help you manage the impact of problems with attention, memory, and thinking clearly, such as adjusting your expectations and letting others help you.
Managing activities of daily living
It is important to become active again when you are recovering, but this can be hard if you feel very tired, breathless, and weak, which is normal after being severely unwell. Everything we do, including washing, dressing, and preparing meals, as well as work and play, takes energy.
After a severe illness, you may not have the same energy you used to, and some tasks may take more effort than before.
If you feel like this, the following strategies may be helpful:
- Adjust your expectations for what you can do in a day. Set realistic goals based on how you are feeling. When you are very tired, breathless, or weak, even getting out of bed, washing, and dressing can be achievements.
- Save your energy by doing tasks sitting down when you can, such as when showering, dressing, or preparing food. Try not to do tasks that need you to stand, bend down, reach high, or squat for a long time.
- Pace yourself and try to do light tasks between heavier ones. You may need to leave yourself time during the day to rest.
- Let others help you with tasks that you may be struggling with. Things like caring for children, shopping, preparing meals, or driving may be difficult. Accept offers of support and let people know what they can help you with. Services that can help with activities, such as shopping or cooking, may also be useful while you are still recovering.
- Ease back into activities. Do not try to take up full activities until you feel ready. This may mean talking to an employer about a gradual return to work, taking on a role that is easier for you to manage, getting support for childcare, and returning to hobbies slowly.
Managing stress, anxiety, or depression
Being extremely unwell in hospital can be a highly stressful experience. This can have an understandably difficult impact on your mood. It is not unusual to experience feelings of stress, anxiety (worry, fear), or depression (low mood, sadness). Memories or dreams of being in the hospital may come to you even if you do not want them to. You may notice difficult thoughts or feelings related to your survival. Your mood may be further affected by frustrations about not yet being able to return to your daily activities the way you would like to.
In turn, these difficult feelings can affect your ability to engage with daily activities- particularly if you are less motivated because of the difference between your expectations and what is achievable.
Managing stress and feelings of anxiety and depression are therefore an important part of your overall recovery.
There are some simple things you can do.
Take care of your basic needs
- Get enough quality sleep. Your sleep was likely disrupted during the hospital. Feeling stressed can also affect your sleep. Try to return to a regular sleeping and waking time, using alarms to remind you. You or your family/carers can ensure that your environment is free from things that might disturb you, such as too much light or noise. Minimizing nicotine (such as from smoking), caffeine, and alcohol and adding relaxation strategies will help you with falling and staying asleep.
- Eating sufficiently and healthily is important for your overall wellbeing. If you struggle with eating or swallowing, follow the advice provided in this leaflet or by a healthcare professional. Family/carers can try to ensure that sufficient food is available to you.
- Be physically active as this reduces stress and can reduce the chance of depression. Take small steps in gradually and safely increasing your physical activity.
Self-care
- Staying socially connected is important for your mental wellbeing. Talking with others can help to reduce the stress and may also help you in finding solutions for challenges in your recovery journey. If you are living alone, staying in contact with friends or family on the telephone or online can help you to feel less alone. Because you may not feel like being socially connected when your mood is low, let family and friends know that they can help by reaching out to you during your recovery.
- Do relaxing activities that do not make you too tired, like listening to music, reading, or spiritual practices. Slow breathing also helps to reduce stress and is another example of a relaxation strategy. These should be done gradually if it is too difficult at first. Follow the “Controlled Breathing Exercises” described earlier in this leaflet to learn how to do slow breathing.
- Gradually increase your involvement in your daily activities or hobbies to the best of your ability, as this helps to improve your mood.
If you were previously receiving services to support your mental health, talk to your provider to ensure that these continue. Family/carers can also play an important role in supporting people who are physically recovering after being ill but have declining mental health. Family/carers may help them access the support they need when they need it.
When to contact a healthcare professional
The impact of being hospitalized and being seriously unwell can be different for everyone. It is important to contact a health professional, such as a general practitioner, rehabilitation professional, or medical specialist, if:
- There is a change in how breathless you are at rest that does not get better by using the breathing control techniques described in this post.
- You become very short of breath with minimal activity and this does not improve with any of the positions for easing breathlessness described in this post.
- You experience any of the symptoms before or during exercise.
- Your attention, memory, thinking, or tiredness are not improving, making it very difficult for you to do your daily activities, or are stopping you from going back to work or other roles.
- Your mood worsens, particularly if it lasts for several weeks.
SOURCE: World Health Organization. Regional Office for Europe. (2020). Support for Rehabilitation Self-Management after COVID-19- Related Illness. World Health Organization. Regional Office for Europe. https://apps.who.int/iris/handle/10665/333287. License: CC BY-NC-SA 3.0 IGO (Support For Rehabilitation Self-Management After COVID-19-Related Illness)
View/Open: WHO-EURO-2020-855-40590-54571-eng.pdf (2.718Mb)
No related posts.

